The Trauma Gap™
The Trauma Gap™ is the systemic failure between what behavioral science understands about human development and what institutions actually operationalize, resulting in misdiagnosis, burnout, ineffective interventions, and escalating mental health outcomes.
Current research shows:
→ Mental health diagnoses increased 35% (2016-2023)
→ PCPs write 70% of psychotropic medications w/ only 8 hrs of training
→ Teacher burnout is directly connected to managing behaviors.
→ Families are navigating crises they weren't trained for
-
The Trauma Gap™ is the systemic disconnect between what we know about childhood developmental trauma as the foundation of mental health struggles and our complete inability to address it at scale.
Research confirms that adverse childhood experiences (ACEs) drive the majority of mental health diagnoses, yet our systems have no infrastructure to identify, treat, or prevent developmental trauma. Instead, we diagnose and treat symptoms, anxiety, depression, ADHD, addiction, while the fractured foundation remains untouched.
The result: diagnoses rise, treatments provide temporary relief at best, practitioners burn out, and intergenerational trauma cycles repeat.
The cost: Billions spent on interventions that fail because we never address the root cause. Individuals cycle through diagnoses and treatments while systems buckle under demands they were never designed to handle.
-
The Trauma Gap™ emerged from a fundamental flaw: our mental health infrastructure was built to treat diagnosed disorders rather than prevent and heal the developmental trauma that causes them.
For decades, systems focused on symptom management, diagnosing anxiety, depression, and behavioral disorders, while leaving the root cause unaddressed. Even as research confirmed the pervasive impact of adverse childhood experiences, our frameworks couldn't accommodate this knowledge.
Trauma-informed care represented progress, but remained reactive, teaching professionals to recognize triggers and respond with empathy after harm occurs, rather than building environments where developmental roots are understood, preventing perpetuation.
The predictable result: practitioners have become the overwhelmed as ‘Mental Health First Responders’ without adequate training, interventions providing temporary relief while patterns persist, and systems buckling under impossible demands.
The Trauma Gap™ persists because we lack infrastructure to move from reaction to prevention: no diagnostic frameworks for developmental trauma, no workforce training, no payment systems that support this work, and no coordinated implementation across sectors.
-
The gap exists across four critical system failures:
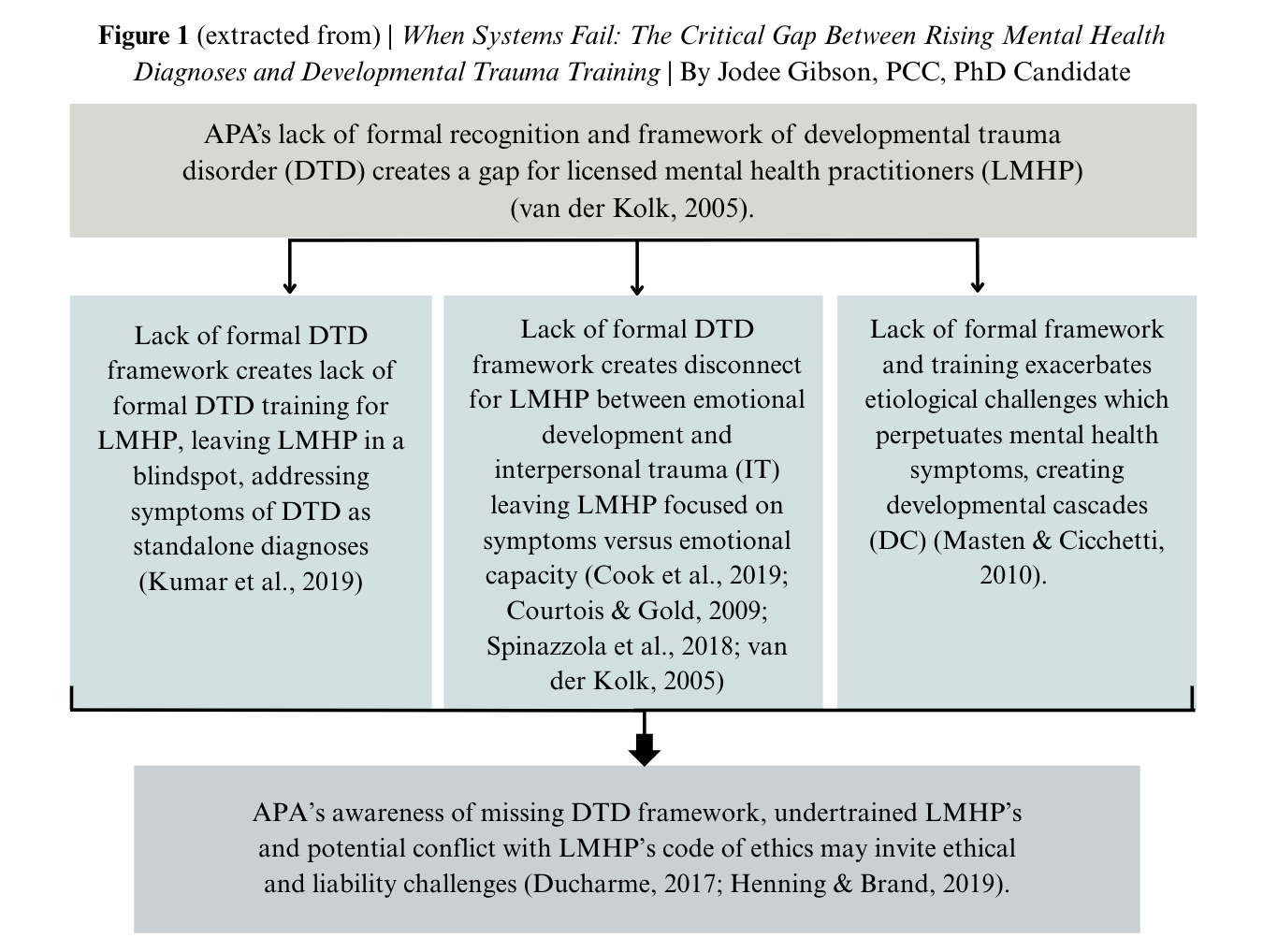
→ Diagnosis | No formal diagnostic framework for developmental trauma exists, forcing practitioners to treat symptoms while the root cause remains invisible and unnamed.
→ Workforce Training | Mental health practitioners are systematically untrained to recognize or treat developmental trauma, despite it being the foundation of most presenting diagnoses.*
→ Treatment Coverage | Insurance providers reimburse licensed mental health professionals for trauma services despite those providers receiving no trauma training, while excluding trauma-trained specialists who could provide effective care.
→ Implementation Infrastructure | Fragmented, siloed systems with no infrastructure to scale or coordinate evidence-based practices across sectors, leaving proven interventions inaccessible.
*While some practitioners pursue trauma training through continuing education, this remains fragmented, inconsistent, and absent from foundational professional training programs.
-
Closing The Trauma Gap™ requires coordinated transformation across policy, workforce development, systems infrastructure, and implementation, moving from a symptom-management approach to one that recognizes, addresses, and heals developmental trauma at its root.
The problem isn’t that we don’t understand trauma.
The problem is that our systems were never built to apply what we know.

Interesting facts abouT trauma
Most people believe these are standalone diagnoses.
→ Anxiety
→ Depression
→ ADHD/ADD
→ Addictions
→ Oppositional Defiant Disorder (ODD)
→ Borderline Personality Disorder (BPD)
→ Substance Use Disorders
→ Eating Disorders
→ Self-Harm & Suicidal Ideation
These are actually symPtoms of unprocessed trauma:
Addressing the root cause and processing what’s beneath it creates space for healing. Once the healing begins, most symptoms naturally dissipate.
Download the Research
(coming soon)
Download our research and dig a bit deeper. | If you are still in the exploratory stage and want dive into the research, it will be available soon. We encourage you to stay connected. We will send it out as soon as it’s available.
The Trauma Gap™ white paper and assessment (coming soon) | Includes framework, research, and the four system failures breakdown.